Parents’ Guide to Teen Depression- Suicide Prevention- Dealing with Cyberbullying
Parents’ Guide to Teen Depression- Suicide Prevention- Dealing with Cyberbullying
16-Aug-2016
Depression goes beyond moodiness.
Temperamental teens are common. But moodiness doesn’t mean depression, Dr. Rubenstein said. Neither does sleeping a lot, which is typical for teens; they actually require more sleep than adults and have trouble falling asleep early.
So how do you know the difference between normal teenage doldrums and depression? Consider if there’s been “a real change in the functioning of [your] child’s behavior,” Strober said. You also might notice changes in appetite and sleep, poor school performance, an inability to concentrate, lack of interest and withdrawal from regular social activities.
“Agitation and irritability in teens may be a sign of depression” as well, according to Rubenstein. However, research hasn’t shown the presence of increased agitation as a distinct symptom, Strober said.
In general, look for consistent patterns. “If depression lasts more than two, certainly three weeks, you want to pay attention,” she said.
1.There’s no quintessential face of depression.
We tend to create categories and stereotypes around certain mental illnesses. That is, many people assume that teens with depression are troublemakers, loners, nerds or artsy types. But depression does not discriminate, Rubenstein noted. It affects all types of teens.
2. Comorbidity is common.
Teens rarely just struggle with depression. “Depressive symptoms are part of a bigger picture,” Rubenstein said. For instance, anxiety commonly co-occurs with depression.
In fact, in her private practice, Rubenstein has noticed more teens coming in with symptoms of anxiety largely because of the combination of academic pressures and attempts to balance school with sports (or other extracurricular activities) and social events. In other cases, depression may be the primary problem, but other disorders, like learning difficulties, still exist.
3. Teen depression is treatable.
Most people think that depression is difficult to treat, Rubenstein said, but treatments like cognitive-behavioral therapy (CBT) can help. According to Strober, research has found that CBT “should be considered as the treatment for mild to moderate depression.” “Between four to six weeks, we can bring some relief,” Rubenstein said.
4. Antidepressants are effective in teen depression
There’s also some evidence that shows certain antidepressants are effective in teen depression. Fluoxetine (Prozac) has shown the most benefit, according to research, Strober said. If the antidepressant is helping, it’s recommended the teen take the medication for a year, he said. Whether medication is necessary “really depends on the seriousness and persistence.
When treating depression in teens, Rubenstein helps her clients create a toolbox to cope with life. Her first goal is to “actively do something that’s helpful to them to give the message that I want to help you where it hurts.” She does this by finding out one change that will relieve the teen’s pain. For instance, if a teen is super stressed at school, dropping one class and picking it back up in the summer may be a reasonable option. In addition to empowering the client, she also lets them know that they can improve, that they don’t have to feel this way.
How Parents Can Help a Depressed Teen
Again, “Teens who are suffering from depression can be helped,” Rubenstein said, so it’s important to get them treatment. If you think your teen has depression, seek a psychologist who specializes in treating adolescents. It’s key to see an expert. As Rubenstein said, “you wouldn’t hire a plumber to put on your new roof.” Even if your teen doesn’t want to go to therapy or you haven’t discussed the option yet, an appointment is critical. A psychologist can educate you on depression (also consider checking out sources on your own), how to help and give you the tools you need.
Similarly, if medication is going to be considered as part of a treatment plan, try to find a psychiatrist who treats children and adolescents. Sometimes, psychologists and psychiatrists will work as a team. For instance, Rubenstein has worked with the same psychiatrist for years. A team approach is important. “This way everyone is on the same page,” she said. Also, your family doctor might be able to recommend a psychologist or psychiatrist.
Parents Can Make a Difference
Every day, about 12 youth die by suicide. For every adolescent death by suicide you hear about, about 25 suicide attempts are made. These are staggering statistics. We know that families, schools, peer groups and communities are dramatically impacted when young people engage in suicidal behavior. We want to help you prevent these tragedies.
Parents can help prevent suicide by recognizing warning signs, identifying risk factors (characteristics that may lead a young person to engage in suicidal behaviors), promoting protective factors (characteristics that help people deal with stress and reduce their chances of engaging in suicidal behaviors), and knowing how to talk to their children and seek mental health services. You can empower yourself and your teen by following these 7 steps.
- Know your facts
Information is power and too much misinformation about suicide can have tragic consequences. Separating myth from fact can empower you to help your teen in distress.
Myth – Suicide in youth is not a problem
Truth – Suicide is a major problem affecting youth; it is the 3rd leading cause of death among 10-24-year-olds
Myth – Asking about suicide causes suicidal behavior
Truth – Addressing the topic of suicide in a caring, empathetic, and nonjudgmental way shows that you are taking your child seriously and responding to their emotional pain
Myth – Only a professional can identify a child at risk for suicidal behavior
Truth – Parents and other caregivers often are the first to recognize warning signs and most able to intervene in a loving way
- Recognize the warning signs
Studies who that 4 out of 5 teen suicide attempts are preceded by clear warning signs, so make sure to know them. A warning sign does not mean your child will attempt suicide, but do not ignore warning signs. Respond to your child immediately, thoughtfully and with loving concern. Don’t dismiss a threat as a cry for attention!
- • Changes in personality: sadness, withdrawal, irritability, anxiety, exhaustion, indecision
- • Changes in behavior: deterioration in social relationships and school and/or work performance, reduced involvement in positive activities
- • Sleep disturbance: insomnia, oversleeping; nightmares
- • Changes in eating Habits: loss of appetite, weight loss, or overeating
- • Fear of losing control: erratic behavior, harming self or others
- Know the risk factors
Recognize certain situations and conditions that are associated with an increased risk of suicide.
- • Previous suicide attempt(s)
- • Mental health disorders (depression, anxiety)
- • Alcohol and other substance abuse
- • Feelings of hopelessness, helplessness, guilt, loneliness, worthlessness, low self-esteem
- • Loss of interest in friends, hobbies, or activities previously enjoyed
- • Aggressive behavior
- • Bullying or being a bully at school or in social settings
- • Disruptive behavior, including disciplinary problems at school or at home
- • High-risk behaviors (drinking and driving, poor decision-making)
- • Recent/serious loss (death, divorce, separation, broken romantic relationship,)
- • Family history of suicide
- • Family violence (domestic violence, child abuse or neglect)
- • Sexual orientation and identity confusion (lack of support or bullying during the coming out process)
- • Access to lethal means like firearms, pills, knives or illegal drugs
- • Stigma associated with seeking mental health services
- • Barriers to accessing mental health services (lack of bilingual service providers, unreliable transportation, financial costs)
- Know the protective factors
These factors have been shown to have protective effects against teen suicide:
- • Skills in problem-solving, conflict resolution, and handling problems in a nonviolent way
- • Strong connections to family, friends, and community support
- • Restricted from lethal means of suicide
- • Cultural and religious beliefs that discourage suicide and support self-preservation
- • Easy access to services
- • Support through ongoing medical and mental health care relationships
- Take preventive measures
You are not powerless; you can guard your teen against the possibility of suicide.
- • Interact with your teen positively (give consistent feedback, compliments for good work.)
- • Increase his/her involvement in positive activities (promote involvement in clubs/sports)
- • Appropriately monitor your teen’s whereabouts and communications (texting, Facebook, Twitter) with the goal of promoting safety
- • Be aware of your teen’s social environment (friends, teammates, coaches) and communicate regularly with other parents in your community.
- • Communicate regularly with your teen’s teachers to ensure safety at school
- • Limit your teen’s access to alcohol, prescription pills, illegal drugs, knives and guns
- • Talk with your teen about your concerns; ask him/her directly about suicidal thoughts
- • Explain the value of therapy and medication to manage symptoms.
- • Address your concerns with other adults in your child’s life (teachers, coaches, family)
- • Discuss your concerns with his/her pediatrician to seek mental health referrals
- Talk to your teen about suicide
Talking to your teen about a topic like suicide can seem almost impossible. Have this important discussion with your teen by using these tips.
- • Talk in a calm, non-accusatory manner
- • Express loving concern
- • Convey how important he/she is to you
- • Focus on your concern for your teen’s well-being and health
- • Make “I” statements to convey you understand the stressors he/she may be experiencing
- • Encourage professional help-seeking behaviors (locate appropriate resources)
- • Reassure your adolescent that seeking services can change his/her outlook
- Last but not least, seek mental health services
Mental health professionals can be essential partners in teen suicide prevention.
- a) Take appropriate action to protect your child
- • If you feel that something is “just not right”
- • If you notice warning signs
- • If you recognize your child has many of the risk factors and few of the protective factors listed above
- b) Find a mental health provider who has experience with youth suicide
- • Choose a mental health provider with whom your child and you are comfortable
- • Participate actively in your child’s therapy.
More Blog
Mental health needs to notice in Bangladesh
12-Sep-2024Like other countries Mental health is one of the warning issues in Bangladesh gradually. Though the immense consequences of this... read more
Happiness tips:
02-Apr-2022Happiness is also one of the important aspects of positive psychology and wellbeing. Do something you enjoy every day, e... read more
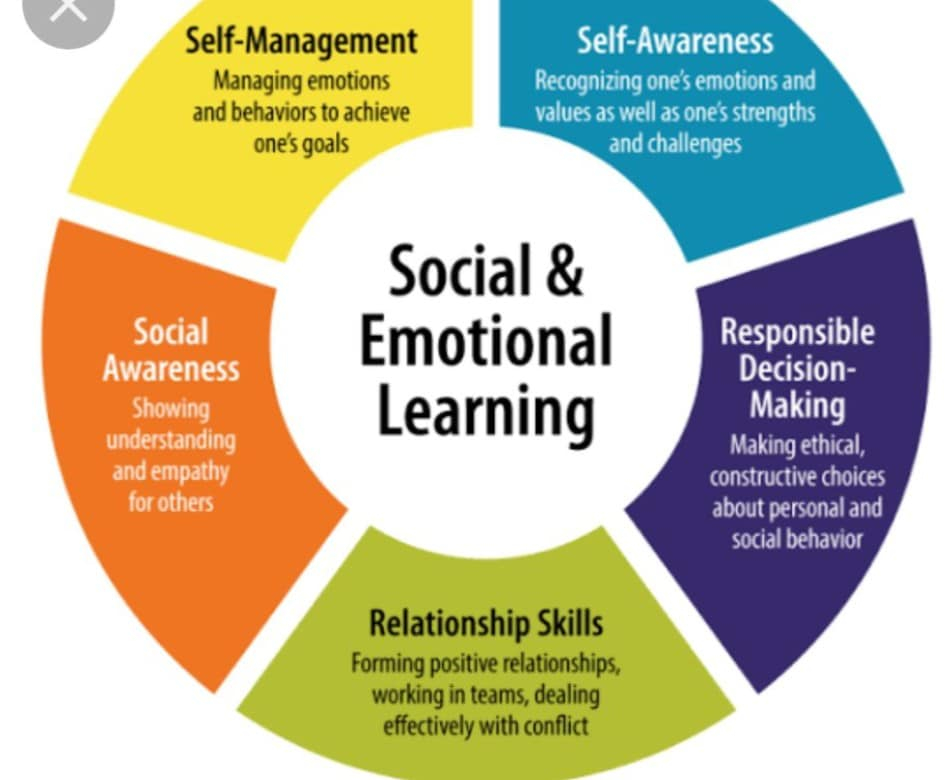
What is SEL?
31-Jan-2022Social-emotional learning, commonly referred to by its acronym, SEL, is a method of promoting holistic child development by teac... read more